GO DEEP WITH EYSUVIS®
(loteprednol etabonate ophthalmic suspension) 0.25%
EYSUVIS® uses AMPPLIFY® Drug Delivery Technology, which is designed to deliver drug particles to the sites of ocular inflammation, where dry eye flares start.1-3
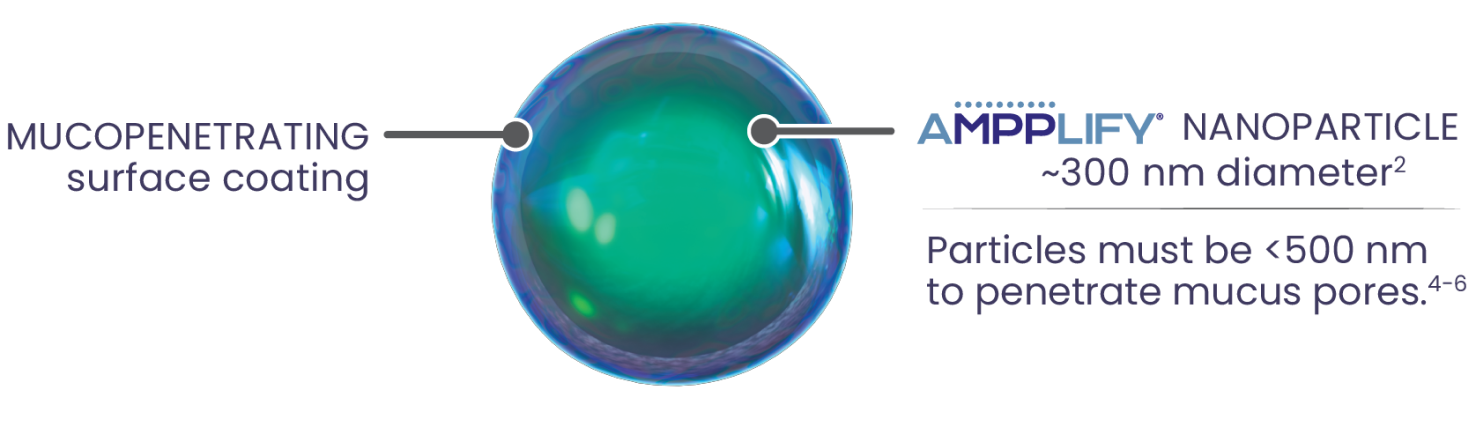
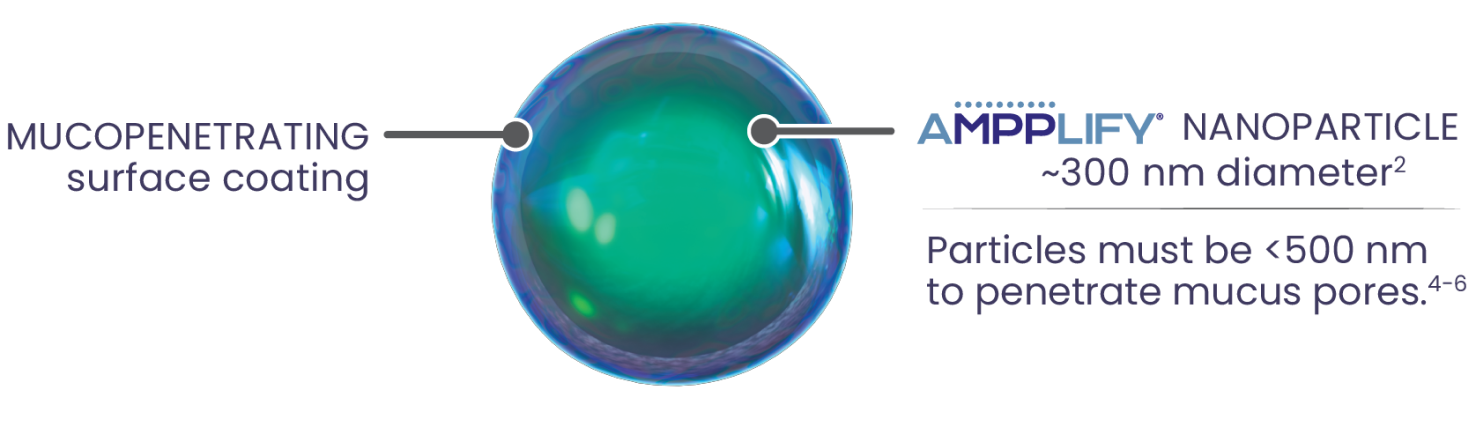
Nanoparticles combined with a mucopenetrating surface coating
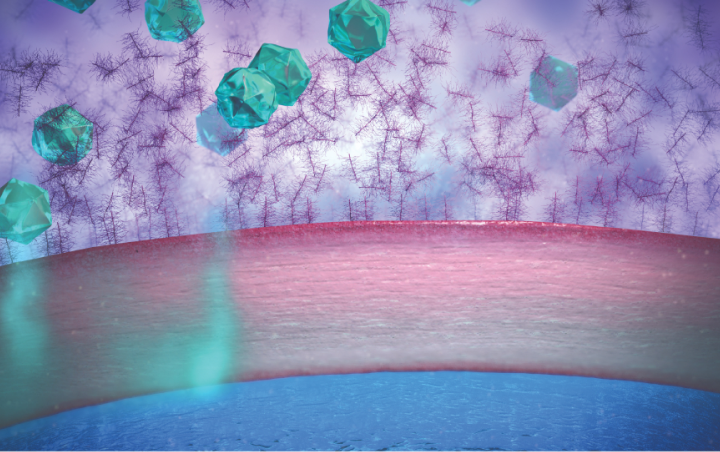
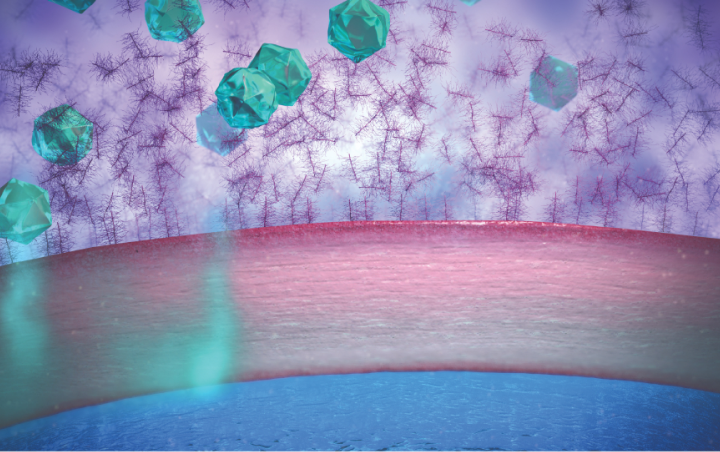
Traditional suspension eye drops adhere to mucins and can be rapidly cleared through blinking1,2
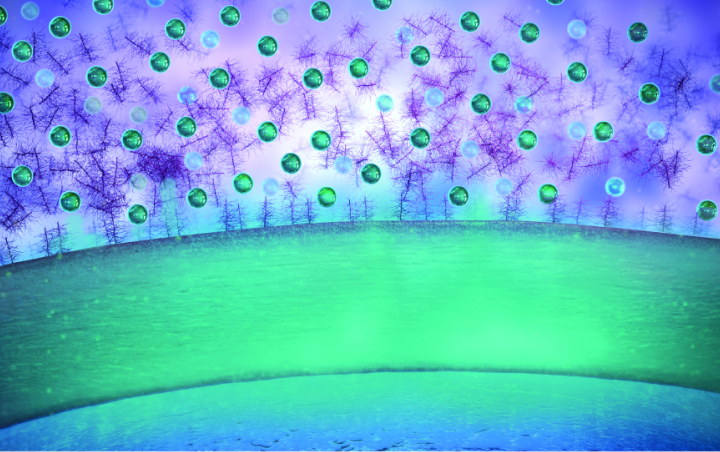
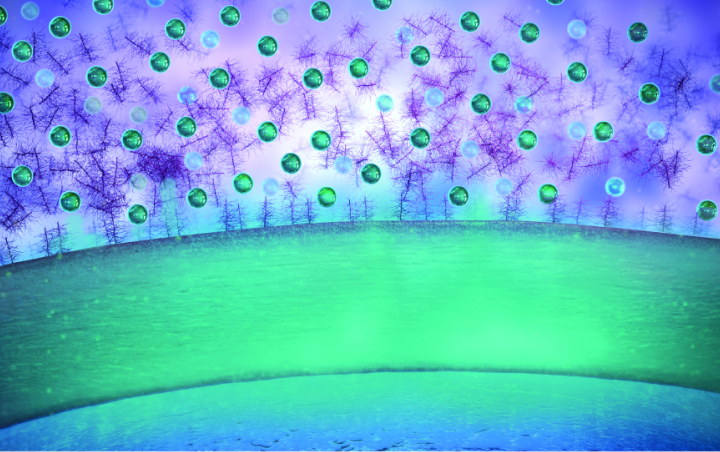
AMPPLIFY® is designed to increase1:
• Ocular surface tissue distribution
• Penetration to the cornea and conjunctiva
REFERENCES
1. Schopf L, Enlow E, Popov A, Bourassa J, Chen H. Ocular pharmacokinetics of a novel loteprednol etabonate 0.4% ophthalmic formulation. Ophthalmol Ther. 2014;3(1-2):63-72.
2. Popov A. Mucus-penetrating particles and the role of ocular mucus as a barrier to micro- and nanosuspensions. J Ocul Pharmacol Ther. 2020;36(6):366-375.
3. Korenfeld M, Nichols KK, Goldberg D, et al. Safety of KPI-121 ophthalmic suspension 0.25% in patients with dry eye disease: a pooled analysis of 4 multicenter, randomized, vehicle-controlled studies. Cornea. 2021;40(5):564-570.
4. Sanders NN, De Smedt SC, Van Rompaey E, Simoens P, De Baets F, Demeester J. Cystic fibrosis sputum: a barrier to the transport of nanospheres. Am J Respir Crit Care Med. 2000;162(5):1905-1911.
5. Sigurdsson HH, Kirch J, Lehr CM. Mucus as a barrier to lipophilic drugs. Int J Pharm. 2013;453(1):56-64.
6. Liu M, Zhang J, Shan W, et al. Developments of mucus penetrating nanoparticles. Asian J Pharm Sci. 2015;10(4):275-282.
IMPORTANT SAFETY INFORMATION
Contraindications
EYSUVIS®, as with other ophthalmic corticosteroids, is contraindicated in most viral diseases of the cornea and conjunctiva including epithelial herpes simplex keratitis (dendritic keratitis), vaccinia, and varicella, and also in mycobacterial infection of the eye and fungal diseases of ocular structures.
INDICATION
EYSUVIS® is a corticosteroid indicated for the short-term (up to two weeks) treatment of the signs and symptoms of dry eye disease.
Warnings and Precautions
Delayed Healing and Corneal Perforation: Topical corticosteroids have been known to delay healing and cause corneal and scleral thinning. Use of topical corticosteroids in the presence of thin corneal or scleral tissue may lead to perforation. The initial prescription and each renewal of the medication order should be made by a physician only after examination of the patient with the aid of magnification, such as slit lamp biomicroscopy, and, where appropriate, fluorescein staining.
Intraocular Pressure (IOP) Increase: Prolonged use of corticosteroids may result in glaucoma with damage to the optic nerve, as well as defects in visual acuity and fields of vision. Corticosteroids should be used with caution in the presence of glaucoma. Renewal of the medication order should be made by a physician only after examination of the patient and evaluation of the IOP.
Cataracts: Use of corticosteroids may result in posterior subcapsular cataract formation.
Bacterial Infections: Use of corticosteroids may suppress the host response and thus increase the hazard of secondary ocular infections. In acute purulent conditions, corticosteroids may mask infection or enhance existing infection.
Viral Infections: Use of a corticosteroid medication in the treatment of patients with a history of herpes simplex requires great caution. Use of ocular corticosteroids may prolong the course and may exacerbate the severity of many viral infections of the eye (including herpes simplex).
Fungal Infections: Fungal infections of the cornea are particularly prone to develop coincidentally with long-term local corticosteroid application. Fungus invasion must be considered in any persistent corneal ulceration where a corticosteroid has been used or is in use.
Adverse Reactions
The most common adverse drug reaction following the use of EYSUVIS® for two weeks was instillation site pain, which was reported in 5% of patients.
View full Prescribing Information for EYSUVIS®.
